Rural Long-Term Care Facilities
Long-term care facilities provide residential living arrangements and a variety of services for people who are unable to live independently at home and may need help with:
- Activities of daily living, such as bathing and getting dressed
- Instrumental activities of daily living, such as preparing meals and shopping for groceries
- Chronic healthcare needs
In addition, long-term care facilities provide patients with the following services:
- Mental or physical rehabilitation
- Nutrition programs and services
- Occupational and physical therapy
- Skilled nursing care
Rural long-term care facilities may include:
- Nursing homes – Provide residential accommodations, help with activities of daily living, and 24-hour skilled nursing care.
- Assisted living facilities – Provide housing and support services to people who need assistance but do not require round-the-clock skilled nursing care. Support may include help with activities of daily living, meals, housekeeping, medication management, transportation, and social and wellness programs.
- Residential services for people with disabilities – Provide housing, nonmedical care, and supportive services for children or adults with disabilities or functional limitations. Many different names are used for facilities of this type, including assisted living, adult living facilities, group homes, developmental homes, community-based residential facilities, and others.
A scarcity of long-term care facilities and healthcare providers in rural communities can cause hardship and difficult choices for individuals and their families. In such cases, people who need long-term care must decide, in consultation with their families and other caregivers, if home care is possible or if relocation to a facility outside of their community is necessary. A move to another community can be stressful, and family members might not be able to visit as often as they would like. Communities also experience economic loss and diminished social connections when people leave.
Frequently Asked Questions
- What services do rural long-term care facilities provide?
- What are the characteristics of residents of rural long-term care facilities?
- Where are long-term care facilities located?
- How is long-term care paid for?
- How does the lack of access to home and community-based services affect utilization of assisted living and nursing homes in rural areas?
- How prevalent is the provision of long-term care services by Critical Access Hospitals?
- What impact do assisted living facilities and nursing homes have on the local economy?
- What types of workforce issues do rural long-term care facilities face?
- What behavioral health needs exist in rural long-term care facilities and how can they be addressed?
- How does the quality of care of rural long-term care facilities compare with other facilities?
- What type of funding is available to build long-term care facilities in rural areas?
- How is technology/telehealth used to meet the needs of those living in long-term care facilities in rural areas?
- What is the role of rural nursing homes in providing post-acute care?
- How are quality initiatives such as antibiotic stewardship implemented in long-term care facilities?
- How are residents' oral health needs met in long-term care facilities?
- How has the COVID-19 pandemic impacted long-term care facilities?
What services do rural long-term care facilities provide?
There is a range of services provided by rural residential long-term care facilities, depending on the needs of the residents at a particular institution and the community. Basic services include living space, nutrition services, housekeeping services, supervised care, medication management, and healthcare coordination. Some also provide physical, occupational, or music therapy; transportation; and social programs and activities.
What are the characteristics of residents of rural long-term care facilities?
Some residents simply need help performing activities of daily living, such as dressing, eating, toileting, and bathing, while others need a higher level of care. According to the University of Minnesota Rural Health Research Center's 2017 policy brief Medical Barriers to Nursing Home Care for Rural Residents, patients in long-term care facilities may suffer from complex, co-morbid medical problems such as obesity, dementia, high blood pressure, and behavioral or psychiatric disorders. In order to address these issues adequately, nursing homes may require extra equipment and staff members who have received advanced training. The researchers found that other possible solutions to these challenges include increased funding, more beds, and elimination of the current Medicare requirement of a three-night inpatient hospital stay to cover post-acute nursing home stays.
The 2019 Certification and Survey Provider Enhanced Reporting (CASPER) data, as reported in the 2022 RUPRI publication Nursing Homes in Rural America: A Chartbook shows that when compared with their counterparts in urban facilities, nursing home residents in micropolitan and noncore areas are more likely to:
- Have their costs reimbursed by Medicaid
-
Have a diagnosis of:
- Dementia
- Psychiatric illness
- Mental or behavioral health needs
- Depression
Nursing Homes in Rural America: A Chartbook also notes that residents of residential care facilities in rural communities not adjacent to urban areas are more likely to be over the age of 85 but less likely to require assistance with certain activities of daily living than residents of urban and urban-adjacent residential care facilities. In addition, Acuity Differences Among Newly Admitted Older Residents in Rural and Urban Nursing Homes notes that rural nursing home facility residents required less complex care than their urban counterparts, but had a higher rate of cognitive impairment and challenging behaviors, such as aggression and wandering.
Where are long-term care facilities located?
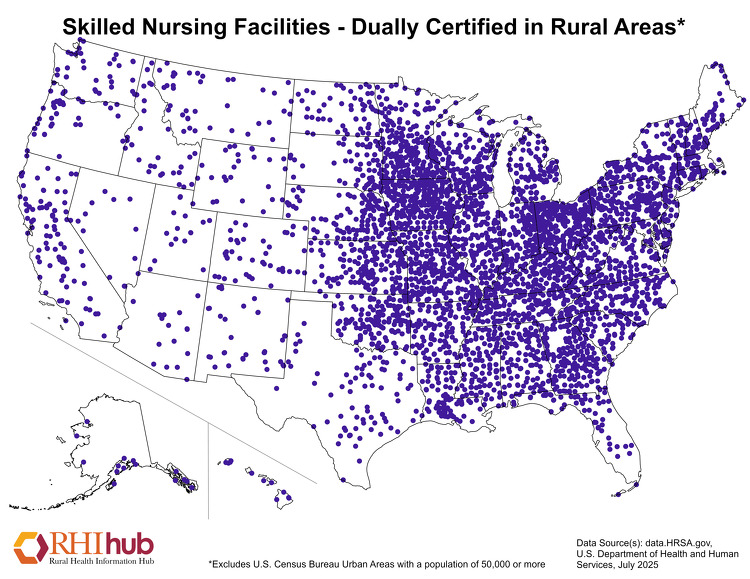
Long-term care facilities are located in rural areas across the United States. The map below shows locations of one type of long-term care facility, dually certified Skilled Nursing Facilities, in rural areas of the country. These institutions have certification both as a nursing facility (NF), which can provide long-term care to Medicaid recipients, and as a Skilled Nursing Facility (SNF), which offers shorter-term rehabilitative care to Medicare recipients. Dually certified facilities can have both "NF beds" and "SNF beds." According to the Skilled Nursing Facility Services chapter of the March 2025 Report to the Congress: Medicare Payment Policy, 27% of all SNFs were in rural areas in 2023.
How is long-term care paid for?
Long-term care can be financed through various public and private sources, each with its own rules on what services are and aren't covered:
Medicaid
Pays for a large share of long-term care services. Patients' assets and income must be below a certain level and
must meet
state eligibility requirements related to the amount of assistance needed. Nursing Homes
in Rural America: A Chartbook notes that Medicaid paid for a higher percentage
of nursing home residents
in micropolitan and noncore counties (63.1% and 64.5%, respectively) compared to residents in metropolitan
counties (57.7%).
Medicare
Medicare provides only short-term reimbursement for care in long-term facilities, and does not cover non-skilled
services related to activities of daily living. According to the Medicare
Payment Advisory Commission, traditional fee-for-service Medicare paid for only 8% of nursing facility
days in the median facility in 2023. Medicare pays for skilled nursing facility care or rehabilitation
services within 30 days following a 3-day hospital inpatient stay, for a maximum of 100 days per benefit period.
Patients are responsible for copays starting on day 21.
For more information on Medicare Part A (Hospital Insurance), see Medicare.gov: Skilled Nursing Facility (SNF) Care.
Veterans Affairs
Veterans are eligible for medical benefits services, which may include long-term care. For specific information,
visit the U.S.
Department of Veterans Affairs Geriatrics and Extended Care: Paying for Long Term Care website.
Commercial Health Insurance
May provide reimbursement for short-term, skilled, medically necessary care in a long-term care facility.
Private Pay
The resident and/or their family pay for services using sources, or a mix of sources, such as:
- Personal savings
- Social Security income
- Family donations
- Long-term care insurance
- Reverse mortgages
- Annuities, pensions, and life insurance options
How does the lack of access to home and community-based services affect utilization of assisted living and nursing homes in rural areas?
In recent years, there has been more emphasis on Medicaid home and community-based services (HCBS) that can allow older adults and people with disabilities to remain in their homes. Preferences for Long-Term Care Arrangements among Rural and Urban Older Adults reports that 62.5% of rural respondents to the 2018 National Health and Aging Trends Study (NHATS) expressed a preference to receive care in their own home, compared to only 31.6% that would prefer to live in an assisted living facility or nursing home. However, Barriers to Aging in Place in Rural Communities: Perspectives from State Offices of Rural Health, explains that access to home care services, access to healthcare, and access to home healthcare are among the barriers State Offices of Rural Health identified to older adults remaining in the community.
Additionally, adequate services may not be available in many rural areas. According to a National Advisory Committee on Rural Health and Human Services 2019 policy brief, when communities lack sufficient home health services and other long-term services and supports, individuals who need long-term care services may have to receive care at "facilities far from their friends and family." In fact, the policy brief Are Rural Older Adults Benefiting from Increased State Spending on Medicaid Home and Community-Based Services?, reports that rural Medicaid beneficiaries were more likely to use nursing facilities than urban Medicaid beneficiaries.
The lack of community-based options may also result in greater burdens for friends and family, as well as lower quality of life for those remaining at home. Caregiving in the US: Rural Family Caregivers, a July 2025 publication from AARP and the National Alliance for Caregiving, notes that family caregivers of older adults living in rural areas often do not live in a rural area themselves and continue to work while serving as a primary caregiver.
For more information on home-based services and community supports in rural areas, see the Community Supports for Rural Aging in Place and Independent Living topic guide.
How prevalent is the provision of long-term care services by Critical Access Hospitals?
In rural communities, Critical Access Hospitals (CAHs) play a vital role in providing long-term care services.
Some CAHs operate Skilled Nursing Facility (SNF) units. Additionally, to increase access to post-acute SNF-level care, the Centers for Medicare and Medicaid Services allows CAHs and other eligible rural hospitals to use swing beds for acute care or post-acute SNF-level care as needed. According to Community Impact and Benefit Activities of Critical Access, Other Rural, and Urban Hospitals, 2022, 40.4% of Critical Access Hospitals offered any long-term care services, including 35.7% that offer skilled nursing care, 11.6% that provide intermediate nursing care, and 5.9% that deliver other long-term care services. In addition, Nursing Homes in Rural America: A Chartbook reports that 52% of all rural hospitals offer nursing facility-type swing beds.
What impact do assisted living facilities and nursing homes have on the local economy?
Assisted living facilities and nursing homes not only serve residents and their families but may also be one of the larger employers in some rural communities. These facilities and their employees contribute to the local economy through local spending for supplies and services, as do friends and relatives who visit facility residents.
The Effect of Nursing Home Closure on Local Employment in the United States found that rural counties experienced a 7.2%-9.4% decline in health sector employment when a nursing home closed. According to the National Center for Rural Health Works' 2017 document The Economic Impact of Rural Nursing Homes, data from a sample of rural nursing homes showed that the facilities surveyed had employment impact of between 70 and 259 employees, and a labor income impact of $3.3 million to $12.0 million when wages, salaries, and benefits were considered. People with various skill levels are needed as workers in these facilities, providing a range of job opportunities for rural residents, including those who may not have medical training.
What types of workforce issues do rural long-term care facilities face?
The National Direct Service Workforce Resource Center's 2011 document Strengthening the Direct Service Workforce in Rural Areas notes that rural long-term care facilities face workforce challenges similar to other rural healthcare facilities. These include:
- Geographic isolation
- Transportation limitations
- Lack of opportunities for training and continuing education
- Chronic provider shortages
- High rates of turnover among staff
Challenges to Admitting Residents: Perspectives from Rural Nursing Home Administrators and Staff summarizes the findings of a 2017 survey of 209 rural nursing home administrators. This study explains that workforce concerns — recruiting, retaining, and training staff, especially with specialized experiences and training — were among the key challenges to providing high-quality care across diverse and complex patient populations. Strengthening the Direct Service Workforce in Rural Areas also notes that long-term care workers often need specialized training, which may be difficult to obtain in rural areas. In such cases, employers must provide the training themselves, or help employees get training in another location or online.
Healthcare workers who are not from rural areas may be disinclined to relocate, thus contributing to the workforce shortage. For this reason, some locations promote grow-your-own programs, in hopes that young people will remain in the area or return there after receiving certification or completing their degrees. For more information, see the Rural Healthcare Workforce and Recruitment and Retention for Rural Health Facilities topic guides.
What behavioral health needs exist in rural long-term care facilities and how can they be addressed?
A 2013 study noted that over the previous twenty years, there had been an increase in the number of nursing home residents with severe mental illness. Many have been diagnosed with dementia, depression, or schizophrenia, and there is a great need for onsite mental health services in long-term care facilities. The 2022 Nursing Homes in Rural America: A Chartbook shows that the percentage of nursing home residents with behavioral and mental health needs, including depression and dementia or Alzheimer's disease, was higher among residents in micropolitan and noncore counties than in metropolitan county in 2019.
The high level of need among nursing home residents who require mental health services is a particular challenge for rural facilities, where there is often a lack of basic mental health infrastructure and significant shortages of mental health professionals. Medical Barriers to Nursing Home Care for Rural Residents highlights that 52% of rural hospital discharge planners interviewed for the study noted that behavioral and psychiatric conditions are the most difficult medical conditions for finding nursing home placements.
In Mental Health Services in Rural Long-term Care: Challenges and Opportunities for Improvement, the authors propose methods for increasing the rural mental health workforce as well as using training programs delivered by telemedicine to build competencies of existing members of the rural health workforce. Using telemental health to provide services to rural nursing home residents is another key suggestion. For one example, see the University of Vermont Medical Center's telepsychiatry consultation service for rural nursing homes.
How does the quality of care of rural long-term care facilities compare with other facilities?
State Actions to Address Nursing Home Staffing During COVID-19, a 2022 KFF issue brief explains that while federal regulations specify minimum staffing levels for certified nursing homes, there is considerable variation in state-level requirements. The 2023 Nursing Home Staffing Study: Comprehensive Report summarizes literature on the relationship between nursing home staffing and quality of care. This report found that higher staff-to-resident ratios are associated with better quality outcomes and that nursing home staff, residents, and family members report quality of care are negatively affected when nursing facilities are short-staffed. While many rural areas have a shortage of RNs and a greater number of older adults within their populations, an August 2020 analysis from the U.S. Department of Health and Human Services Office of Inspector General shows that a lower percentage of rural nursing homes spent at least 1 day below required federal staffing levels than urban facilities.
The 2022 Nursing Homes in Rural America: A Chartbook compares the quality ratings measuring physical and clinical measures of nursing home quality in metropolitan, micropolitan, and noncore areas. A similar percentage of noncore and metropolitan nursing homes received 4 or 5 stars in 2019 (46.2% and 45.1%), while a slightly lower percentage of micropolitan nursing homes (43.2%) received 4 or 5 stars. Meanwhile, only 33.4% of noncore nursing homes received 1 or 2 stars, while greater percentages of metropolitan and micropolitan nursing homes (37.7% and 38.6%) received one of these lower ratings. However, a higher percentage of nursing homes in noncore counties received 4-5 stars in overall survey ratings (40%) than nursing homes in micropolitan and metropolitan counties (33% and 32.7%, respectively).
What type of funding is available to build long-term care facilities in rural areas?
The U.S. Department of Agriculture (USDA) offers a variety of funding opportunities, including direct loans and grants, for construction in rural communities. The Strategic Economic and Community Development Program makes it possible for the USDA to put priority on projects that promote regional economic development through several funding programs. These include:
- Community Facilities Direct Loan and Grant Program
- Community Facilities Guaranteed Loan Program
- Business and Industry Loan Guarantee Program
- Rural Business Development Grants
How is technology/telehealth used to meet the needs of those living in long-term care facilities in rural areas?
Nursing homes in rural areas often do not have 24-hour coverage by physicians, and as a result, patients may sometimes be transferred to a hospital unnecessarily if intervention is needed at a time when a physician is not present. This can result in higher costs and a greater risk of medical complications for patients. However, when telemedicine is used for consultation with off-site medical professionals, the cost is typically lower and patients may have better outcomes. Telehealth Brings Important Services to Rural Long-Term Care Facilities, a 2022 Rural Monitor article, examines the benefits of telehealth services for long-term care facility residents and staff. 2021 Long-Term Support Services Telehealth Results Summary notes that telehealth also helped prevent disease transmission during outbreaks and increase cooperation between physicians, nurses, and patients during the COVID-19 public health emergency.
An Evaluation of Telehealth Expansion in U.S. Nursing Homes, a 2021 study examining telehealth use in nursing homes nationwide, found that larger metropolitan nursing homes reported greater use of telehealth services than smaller and rural facilities. In addition, 2021 Long-Term Support Services Telehealth Results Summary outlines barriers to telehealth use in nursing homes, including different healthcare systems and facilities using different platforms, potential scheduling and staffing issues, reimbursement concerns, and patients' functional limitations.
The Long-Term Care Nursing Homes Telehealth and Telemedicine Tool Kit from the Centers for Medicare & Medicaid Services (CMS) offers resources to aid long-term care facilities in developing a telemedicine program. For an example of successful telehealth use in a rural nursing home, see the University of Vermont Medical Center's Nursing Home Telepsychiatry Service.
What is the role of rural nursing homes in providing post-acute care?
Patients who need extra help when recuperating after hospital discharge often find that a temporary stay in a nursing home is ideal for their needs. They may require wound care, IV medications, feeding tubes, dialysis, rehabilitation or occupational therapy or other specialized care. In this situation, the expectation would be that the nursing home stay would be of limited duration, and the patient would return to his or her previous living situation after healing and regaining strength. However, Post-Acute Care Trajectories for Rural Medicare Beneficiaries: Planned versus Actual Hospital Discharges to Skilled Nursing Facilities and Home Health Agencies, a March 2021 policy brief from the WWAMI Rural Health Research Center, found that while 19% of hospitalized rural Medicare beneficiaries had a planned discharge to a skilled nursing facility (SNF) in 2013, only 16.9% were admitted to a SNF.
Post-acute care in rural areas may also be provided in hospitals with fewer than 100 licensed beds that have received CMS approval to participate in the Medicare swing bed program. Under this arrangement, beds may be used, as needed, either for acute care or for post-hospital skilled nursing care. Nursing Homes in Rural America: A Chartbook reports that 61% of all rural hospitals, including Critical Access Hospitals, offer swing beds. For more information, see the North Carolina Rural Health Research Program's policy brief, Discharge to Swing Bed or Skilled Nursing Facility: Who Goes Where? and the What is a swing bed? section of the Critical Access Hospitals (CAHs) topic guide.
The Rural Monitor article Rural Post-Acute Care: Improving Transitions to Enhance Patient Recovery gives examples of the ways in which rural residents can benefit from post-acute care provided by skilled nursing facilities and other providers.
How are quality initiatives such as antibiotic stewardship implemented in long-term care facilities?
According to the 2018 article Nursing Home Infection Control Program Characteristics, CMS Citations, and Implementation of Antibiotic Stewardship Policies: A National Study, infection control is a priority in long-term care facilities for the following reasons:
- Shared dining and recreational spaces increase the risk of transmitting disease.
- Residents experiencing cognitive decline may not be able to communicate disease symptoms to staff.
- Residents often have underlying health conditions that make infections more dangerous.
- Historically, many nursing home infection prevention programs have suffered from problems such as inadequately trained staff and high turnover rates.
- Clinicians may not be available when infection management decisions need to be made.
To address these risks, CMS requires that nursing homes employ a trained infection preventionist whose main responsibility is infection control, and have in place an infection control program with an antibiotic stewardship component. The CDC document The Core Elements of Antibiotic Stewardship for Nursing Homes describes practical ways for nursing home staff to initiate or expand antibiotic stewardship activities. These include:
- Leadership Commitment – Demonstrating support for appropriate antibiotic use
- Accountability – Identifying which staff members are responsible for overseeing stewardship activities
- Drug Expertise – Establishing access to pharmacists or people with experience in this area
- Action – Implementing one or more policy or procedure to improve antibiotic use
- Tracking – Monitoring one or more measures of antibiotic use and one or more outcomes from antibiotic use in the facility
- Reporting – Providing feedback on a regular basis to relevant staff members
- Education – Making resources available so that clinicians, nursing staff, patients, and families can learn about antibiotic resistance and ways to improve antibiotic use
The CDC offers additional documents to help promote antibiotic stewardship in nursing homes, including:
- Checklist: The Core Elements of Antibiotic Stewardship for Nursing Homes
- Appendix A: Policy and Practice Actions to Improve Antibiotic Use
- Appendix B: Measures of Antibiotic Prescribing, Use and Outcomes
- Appendix C: Data Sources, Elements, and Measures for Tracking Antibiotic Use in Nursing Homes
How are residents' oral health needs met in long-term care facilities?
The 2016 report Evolving Delivery Models for Dental Care Services in Long-Term Care Settings: 4 State Case Studies notes that dental services in nursing homes are limited, despite the fact that residents tend to have poorer oral health than people who live independently. Medicaid and Medicare regulations specify that LTC residents enrolled in these programs have access to basic dental care supplies and must have a dental assessment, but this can be done by nursing staff rather than by a dental professional. There are few, if any, certification requirements specific to oral healthcare providers working in long-term care facilities.
There are practice models being implemented in some rural locations that help with provision of oral healthcare to underserved long-term care facilities. These include:
- Use of mobile equipment, so that patients need not be transported to a dental office
- Telehealth technology
- Rotations for dental students in LTC settings
- Continuing education courses in geriatric oral care
- Collaborative practice models between dentists and dental hygienists or therapists, where allowed
Programs like Missouri's Oral Health Alliance help increase access to oral health services for LTC patients by reaching out to dentists, hygienists, and local health departments who can then provide screenings and healthcare at LTC facilities. The Alliance also educates caregivers by showing them effective oral healthcare techniques and teaching them how to spot cavities and mouth sores.
The National Rural Health Association's 2013 policy brief Rural America's Oral Health Care Needs recommended that access to oral health services be improved for residents of rural long-term facilities by increasing Medicaid reimbursement for dental work, making the administrative burden of participation in the program less cumbersome, and providing reimbursement for procedures instead of reimbursement per visit.
How has the COVID-19 pandemic impacted long-term care facilities?
Nursing home and other congregate long-term care facility residents are especially vulnerable to infectious disease, including SARS-CoV-2, the virus responsible for COVID-19. By its nature, long-term care requires staff to have close, direct contact with residents, increasing the risk of the spread of infection throughout a facility. Outbreaks of the disease in nursing homes have resulted in high rates of morbidity and mortality largely due to residents' high prevalence of risk factors, including advanced age and underlying health conditions. The spread of infection also exacerbated the existing strain on the rural nursing home workforce. A December 2022 Government Accountability Office (GAO) analysis found that, prior to the introduction of COVID-19 vaccines, the length of an outbreak in a nursing home was strongly associated with community transmission, facility size, staffing shortages, and ownership type.
In response, the Centers for Disease Control and Prevention (CDC), Centers for Medicare and Medicaid Services (CMS), and state Medicaid agencies provided flexibilities for long-term care facilities during the COVID-19 Public Health Emergency (PHE). For example, CMS expanded the ability of healthcare providers, including nursing homes, to deliver services via telehealth through 1135 waiver authority and modified quality reporting requirements. Guidance for the Expiration of the COVID-19 Public Health Emergency (PHE) outlines the emergency waivers related to the minimum health and safety requirements for long-term care and acute continuing care providers that expired at the end of the PHE and details the timelines for policies that have been modified by the end of the PHE or extended through December 2024 through legislation. See the COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers and Guidance for the Expiration of the COVID-19 Public Health Emergency (PHE) for information on changes to regulatory waivers and flexibilities relevant to long-term care providers implemented during the PHE.

