Arkansas Rural Health Partnership Hospital-based Transitional Care Program
- Need: Solutions for Medicare beneficiaries' post-acute care recovery gaps in Arkansas's southeast Delta Region.
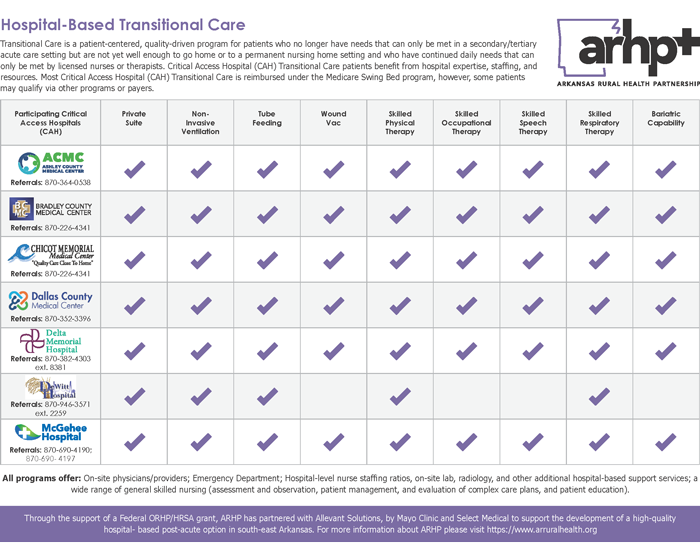
- Intervention: Supported by federal funding and their membership organization, seven hospitals implemented an evidence-supported Critical Access Hospital transitional care model.
- Results: Participating hospitals found a significant increase in swing bed services revenue, an all-cause low readmission rate, high percentage of patients discharged to home or to an assisted living environment, and positive patient satisfaction surveys.
Evidence-level
Promising (About evidence-level criteria)Description
Transitional care (TC), with its focus on "the right care, at the right place, at the right time," is more formally defined by the Centers for Medicare and Medicaid Services (CMS) as transitions of care, referring to the movement of a patient from one setting of care — such as hospitals, ambulatory primary or specialty care practices, long-term care, home health, or rehabilitation facilities — to another. For decades, rural healthcare leaders, rural health researchers, and other professionals have explored solutions to rural TC gaps.
Evidence suggests that when rural hospitals can accept post-acute care admissions from a tertiary hospital, the tertiary hospital has increased bed availability and is more able to accept rural patients needing tertiary care, especially during times of high regional demand like that experienced during the COVID-19 pandemic.
To promote Critical Access Hospitals' (CAHs) ability to meet the TC needs of rural patients, a specific CMS reimbursement model — referred to as swing bed services payment — is available that covers TC provided by a CAH's nursing and rehabilitation resources, other onsite medical providers, and pharmacy, lab, and radiology services. Data also suggests that for many reasons, the CAH swing bed option is underutilized, leaving gaps in TC for rural Medicare beneficiaries across the country.
To close this gap, the Arkansas Rural Health Partnership (ARHP) leveraged a 2020-2023 Federal Office of Rural Health Policy (FORHP) Rural Health Care Coordination Program grant and used a regional programmatic approach to implement swing bed TC in the southeast Arkansas Delta.
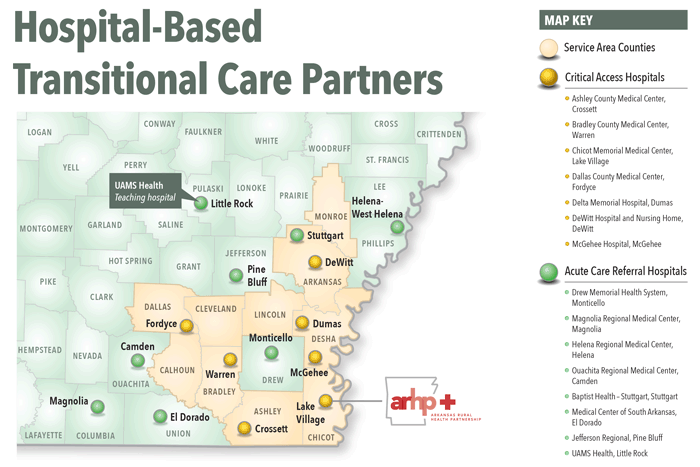
ARHP is 23-member organization of rural-serving hospitals, Federally Qualified Health Centers, and medical schools with a mission to advance the health and wellness of rural residents, providers, and healthcare organizations "through dynamic collaboration, forward-thinking, and the strategic leveraging of resources."
Project goals were accomplished with assistance from a consulting group and their CAH TC care model that was originally developed in 11 CAHs in Minnesota, Wisconsin and Iowa. Now implemented in about 10% of the country's 1,300-plus CAHs, the model's benefits are linked to improved financial and quality outcomes.
To address the many moving parts of bidirectional patient flow, ARHP's grant-funded project had several objectives:
- Plan and disseminate an evidence-supported and sustainable CAH TC program
- Educate and support partner hospital leaders, providers, and staff in developing a high-quality, post-acute TC process
- Increase awareness of TC options for the specific Delta area's rural and urban hospitals
To maximize each CAH site's experience, the project involved a collaborative implementation approach. For example, because the ARHP project director had established relationships and knowledge of each participating hospital's unique challenges, they were able to provide the consulting team with general oversight and assistance that fostered connections between the consulting group and the participating hospitals, allowing the consulting team to tailor and adapt recommendations during the effort.
ARHP also connected with the region's tertiary care hospitals, while the consulting team worked virtually with CAH project managers to implement and integrate the model's "hard-wired success components." These components ranged from proprietary education modules — including those used to bridge experience-complexity gaps — to assistance in revision or creation of policies, procedures, and practices; and program data tracking and analysis.
Health and well-being education and resources were available to participating CAH team members through the consultant's module and materials, with the option for patient use during their TC stay. Also, weekly communication between CAH staff and larger hospitals' discharge planners allowed discussion around both CAH capacity and the regional hospitals' discharge needs.
Because the project was implemented during the COVID-19 public health emergency (PHE) and all hospitals in the southeast Delta region were functioning in crisis mode, additional insights into the power of CAH TC surfaced. An early decision made by ARHP and participating site leaders was to continue the project as the pandemic was creating an even greater need for solid care transition programs. Additionally, the consulting team provided a consistent presence as the pandemic drove the reassignment and departures of many individuals serving in multiple administrative and clinical roles at the participant rural CAHs and Delta region tertiary facilities.
Program outcomes included not only the importance of having CAH TC in place to meet the healthcare needs of rural populations during a PHE, but participating organizations realized increased swing bed revenues, low discharge rates back to acute care from a TC stay of 30 days or less, and a high percentage of patients discharged back to their homes or to an assisted living environment.
Noting that the grant support concluded in August 2023, as of July 2024, the original seven participating CAHs continue to offer CAH TC.
Services offered
Roles and services continuing since program CAH-based TC program model implementation:
ARHP:
- Continuing conversations with regional acute care hospitals to support recognition of the CAH-based TC benefits at member sites
Rural/CAH roles, services, and processes continuing at some ARHP sites:
- Continued provision of quality local TC services
- Continued use of transfer workflows specific to each CAH and tertiary care providers
- Continued communication with facilities providing higher level of care
- Examples of continued ongoing data analysis at each
CAH:
- Swing bed revenue
- Patient transfers to higher level of care
- Patient transfers for recovery services
- Recovery length of stay
- Readmissions
- Discharge disposition (home, custodial care, ongoing care for skilled needs)
Results
Results from the original grant-supported activity were:
Targeted support, training, and assistance to equip CAHs to care for not only more patients, but more complex patients as indicated by these results:
- Increased use of existing rural CAH resources for post-acute recovery
- An overall 20% increase in swing bed revenues
- Shorter average transition care length of stay as
compared to the 2022 national Medicare Part A nursing
home average
- Approximately 12 days as compared to 28 days
- Low likelihood of discharge back to acute care
setting from the TC setting
- Demonstrated by 8% discharge from CAH TC back to acute setting (including planned and unplanned) for patients with a CAH TC stay of 30 days or less
- High percentage of discharge back to independent or
assisted-living settings
- Around 70% of admitted patients discharged back to home or assisted-living
- More than 75% of patients who lived at home or assisted living prior to their acute stay returned to home or assisted living
- Three of the pilot CAHs used a 9-question patient
satisfaction survey
- Of 130 respondents, average ranking per question was ranged from 4.77 to 5.0 on a 5-point scale
Additional subjective results:
- CAH administrative leadership:
- Gained awareness of how a focus on staff health and wellness can improve long-term staffing stability
- CAH internal team changes:
- Increased confidence in the post-acute recovery care of complex patients
- Enhanced internal communication
- Enhanced teamwork in delivering CAH-TC patient care
- Increased external communication with tertiary care hospitals
During the project, several CAHs updated program brochures and web content geared to increasing community awareness about local recovery care services. ARHP created a CAH capabilities summary handout as a reference for the region's acute care hospitals.
Challenges
For all grant participants, innumerable challenges were directly related to delivering rural healthcare during a pandemic. Examples were staffing shortages with some CAHs relying on high-cost travel nurses for over 50% of their nurse staffing at times. CAH nurses leaders and project support staff were often called to the bedside or moved to other PHE priority efforts such as vaccination clinics.
At tertiary care centers, case managers often lacked familiarity with CAH TC availability due to frequent staff turnover.
Messaging around the provision of CAH TC was also impacted. Project leaders believed that although there was increased understanding of the breadth and benefits of the CAH TC available in their rural communities, messaging was overshadowed significantly by COVID-19 education and information.
Replication
Recommendations for organizations interested in implementing a dedicated CAH TC include:
- Gain and maintain CAH senior leadership support
- Build and maintain relationships with the region's healthcare systems
- Embrace adaptability
- Anticipate slow progress and elevate progress as positive
- Demonstrate value by collecting outcome data
- If able, engage experienced experts to support quicker and more effective program development and growth
Contact Information
Lynn Hawkins, Chief Operations OperatorArkansas Rural Health Partnership
501.588.3938
lynnhawkins@arruralhealth.org
Topics
Access
· Aging and aging-related services
· Care coordination
· Critical Access Hospitals
· Delta Region
· Healthcare networks
· Healthcare quality
· Medicare
· Networking and collaboration
· Post-acute care
· Reimbursement and payment models
· Swing bed services
States served
Arkansas
Date added
July 26, 2024
Suggested citation: Rural Health Information Hub, 2024 . Arkansas Rural Health Partnership Hospital-based Transitional Care Program [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1144 [Accessed 12 December 2025]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
