ROAMS (Rural OB Access & Maternal Service)
- Need: To improve maternal health in northeastern New Mexico.
- Intervention: The Rural OB Access & Maternal Service program provides obstetric and maternal fetal medicine telehealth, home telehealth kits, and free access to lactation consultants and family navigators.
- Results: ROAMS has worked with 2,000 unique individuals since July 2021.
Description
 In
northeastern New Mexico, many patients face
barriers to maternal health including poverty, long
drives to appointments, and local providers unable to
care for high-risk pregnancies. To improve maternal
health, Holy Cross Medical Center in Taos, Miners Colfax
Medical Center in Raton, and Union County General
Hospital (UCGH) in Clayton created the ROAMS (Rural OB Access &
Maternal Service) program. ROAMS provides obstetric and
maternal fetal medicine telehealth, home telehealth kits,
and free access to lactation consultants and family
navigators.
In
northeastern New Mexico, many patients face
barriers to maternal health including poverty, long
drives to appointments, and local providers unable to
care for high-risk pregnancies. To improve maternal
health, Holy Cross Medical Center in Taos, Miners Colfax
Medical Center in Raton, and Union County General
Hospital (UCGH) in Clayton created the ROAMS (Rural OB Access &
Maternal Service) program. ROAMS provides obstetric and
maternal fetal medicine telehealth, home telehealth kits,
and free access to lactation consultants and family
navigators.
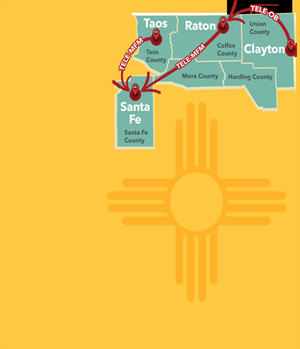
ROAMS serves the following rural counties:
- Colfax
- Harding
- Mora
- Taos
- Union
ROAMS received a 2019-2023 Federal Office of Rural Health Policy (FORHP) Rural Maternity and Obstetrics Management Strategies (RMOMS) grant and is currently funded by the Conrad N. Hilton Foundation, the Brindle Foundation, and the Managed Care Organization Reinvestment Fund through the state's Medicaid program.
Services offered
Patients can use telemedicine to connect with obstetricians (OBs), and those with high-risk pregnancies can connect to maternal fetal medicine (MFM) providers in Santa Fe or Albuquerque.
ROAMS patients can receive a home telehealth kit that allows them to complete telehealth appointments at home and measure vital signs like blood pressure and fetal heart rate. Patients can also receive texts with information and appointment reminders during their pregnancies and postpartum.
Patients can meet with lactation consultants and with family navigators/community health workers to address social determinants of health like transportation or food insecurity.
Results
 UCGH Health Clinic facilitated 108
tele-OB appointments, saving patients a total of 18,360
miles and 324 hours of driving.
UCGH Health Clinic facilitated 108
tele-OB appointments, saving patients a total of 18,360
miles and 324 hours of driving.
From September 2019 to August 2020, 41% of expectant mothers at Miners Colfax Medical Center did not have a prenatal exam in the first trimester. From 2020 to 2021, that number went down to 36% and then dropped to 25% the following year.
Challenges
It was challenging to establish partnerships between medical organizations that share patients but don't usually collaborate.
Sustaining a tele-OB program can be a challenge since many rural hospitals lose money by providing OB services and don't want to split the billing with another site through tele-OB.
Replication
Rural locations receiving tele-MFM services need a high-quality ultrasound and a trained sonographer. Tele-MFM is more complicated and expensive to implement than tele-OB.
Tele-OB is relatively easier to implement than tele-MFM, since it does not require as much technology or staff training.
Topics
Community health workers
· Maternal health and prenatal care
· Maternal health workforce
· Telehealth
States served
New Mexico
Date added
February 21, 2024
Date updated or reviewed
April 2, 2025
Suggested citation: Rural Health Information Hub, 2025. ROAMS (Rural OB Access & Maternal Service) [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1134 [Accessed 15 April 2025]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
